Zsombor Zrubka health economist and associate professor at Óbuda University was the speaker of the Alumni Hungary Webinar in June. He held an exciting presentation about the role of digitalisation and the use of artificial intelligence in healthcare. We interviewed him about his work, research and the prospects of digital health.
Originally you are a medical doctor. How did you turn into health economics, and what exactly does a health economist do?
In the early 2000s, many physicians left heatlhcare for the pharmaceutical industry in Hungary, which seemed a lucrative and exciting career opportunity. I spent 17 years in the pharma industry in various roles including national and international brand management and business unit management. As the pressure grew on the industry to demonstrate the value of its innovations before entering the market, I realised the importance of health economics. Then I became more and more interested in its intellectual and methodological aspects until I decided to leave the industry behind and become a full-time scholar. Health economics is an interdisciplinary science, focusing mainly on decision-making concerning health or healthcare by individuals, healthcare providers, or governments when facing scarcity of resources.

You are the head of HECON – Health Economics Research Center at Óbuda University. What is the main role of the center, and what type of research do you conduct there?
At HECON our task is to develop a unified research and educational strategy for health economics and technology assessment for Óbuda University. We provide professional support to faculties and university research centers, jointly design and conduct research projects and apply for research grants, which integrate the results of medical, technical, economic and business sciences. Currently, our main focus is on the health economic aspects of digital technologies in healthcare. More specifically, we perform evidence syntheses of digital technologies, measure the health outcomes related to digital technologies, and study the economic and societal impact of digital technologies in healthcare.
Digitalisation affects healthcare in many ways, but what could be its role for hospitals? How can digital technologies improve the services of hospitals?
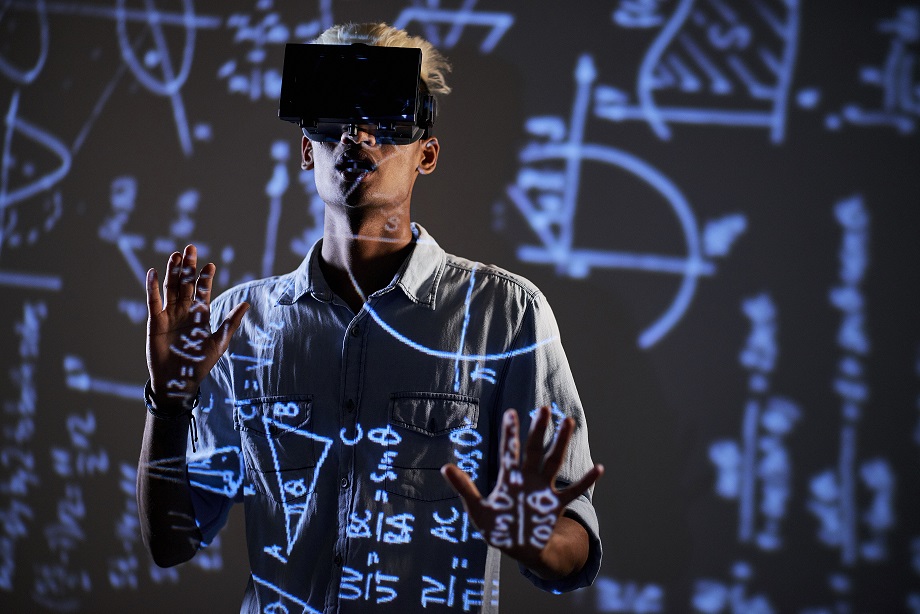
Digitalisation is ubiquitous, it is present everywhere in our lives. By making information cheaper and more accessible, it can transform nearly every activity that is being conducted in a hospital. It would be difficult to give a comprehensive list, but from using virtual reality tools to aid surgeons through artificial intelligence-driven decision support or diagnostic systems to a variety of tools that aid the administrative and logistical tasks in a hospital, I can imagine a very long list. And these systems can connect with other systems within and outside the hospital, improve the information about the patient or optimise the patient-pathway between various stages. And these real-world data could then feed directly into real-world clinical trials and safety databases to advance science. Of course, we need to be aware of the data protection and data privacy regulations and the cybersecurity risks involved with such systems. And we need to make more transparent and interpretable how artificial intelligence algorithms give recommendations, to avoid hidden errors or algorithmic biases. And we need to tackle ethical and legal issues concerning professional responsibility. Therefore, I think, although the potential is huge, it will take time until all the benefits of digital technologies can be realised.
In your presentation, you mentioned that there are more than 400.000 mobile health apps available. How can we make sure without expert knowledge which apps are truly reliable?
It is a difficult question. Information overload and scarcity of attention is a problem for professionals and patients as well in the digital world. In the first place, one should look for the CE mark, which indicates that the app has been authorised by a regulatory agency. Some professional organisations also review and authorise apps before they are implemented in health systems. Patients should consult their doctors or other healthcare professionals because most probably they will have experience with the apps that have true medical benefits. And e-Health literacy can help patients to get the information and assess if it is realiable, from a variety of clues. But despite all of this, there is no guarantee that an app will work for a given patient. Some apps are based on proven psychological or behavioural theories, while others are more naïve in this sense. Beyond the intended benefits, the user experience also influences if the app will eventually work. Most of the healthcare apps are used only a few times and only a fraction of them are being used on a regular basis.
What do you think about the use of ChatGPT in healthcare? How reliable is it right now, and in which directions can it develop to in terms of health?
This is a difficult question. ChatGPT was a leap in technology, which became a surprise for many of us. ChatGPT is a large language model, which has been trained to conduct human-like conversations. It has not been developed for healthcare, but it may be possible to further develop for heatlhcare uses. But healthcare products are regulated products, only those products can be used for medical purposes, which have been authorised by a regulatory agency. This means that there is sufficient scientific proof that the benefits of a technology outweight its risks when used in healthcare. I think the complexity of ChatGPT is one feature that makes it very difficult for authorities to deal with. Therefore, I think, transparency, quality assurance, safety and regulatory standards, and medical evidence on the benefits and risks are prerequisites for using ChatGPT in healthcare.